A few years ago, a young man from California’s technology scene began popping up in the world’s leading developmental biology labs. These labs were deciphering the secrets of embryos and had a particular interest in how eggs are formed. Some thought if they discovered that recipe, they would be able to copy it and transmute any cell into an egg.
Their visitor, Matt Krisiloff, said he wanted to help. Krisiloff didn’t know any biology, and he was only 26. But after leading a research program at Y Combinator, the famous startup incubator in San Francisco that was an early funder of such companies as Airbnb and Dropbox, he said, he was “well connected,” with access to wealthy tech investors.
Krisiloff also had a specific interest in the artificial-egg technology. He’s gay, and he knew that theoretically, a cell from a man could be turned into an egg. If that were ever possible, two men could have a child that was genetically related to both. “I was interested in the idea of ‘When can same-sex couples have children together?’” says Krisiloff. “I thought that this was the promising technology for doing this.”
Today the company Krisiloff started, called Conception, is the largest commercial venture pursuing what’s called in vitro gametogenesis, which refers turning adult cells into gametes—sperm or egg cells. It employs around 16 scientists and has raised $20 million from well-known tech figures including Sam Altman, the CEO of OpenAI and former president of Y Combinator; Jaan Tallinn, one of the founders of Skype; and Blake Borgeson, a cofounder of Recursion Pharmaceuticals.
The company is initially trying to make replacement eggs for women. That’s scientifically easier than making eggs from male cells, and it has an obvious market. People are having kids later in life, but a woman’s supply of healthy eggs nosedives in her 30s. It’s a major reason patients visit IVF clinics.
Conception is starting with blood cells from female donors and trying to transform these into the first “proof-of-concept human egg” made in the lab. The company hasn’t done it yet—nor has anyone else. There are still scientific puzzles to overcome, but Krisiloff sent out an email to supporters earlier this year saying his startup might be be “the first in the world to accomplish this goal in the not-too-distant future.” It says that artificial eggs “could become one of the most important technologies ever created.”
That’s no exaggeration. If scientists can generate supplies of eggs, it would break the rules of reproduction as we know them. Women without ovaries—for example, because of cancer or surgery—might be able to have biologically related children. What’s more, lab-made eggs would cancel the age limits on female fertility, allowing women to have related babies at 50, 60, or even beyond.
The prospect of egg cells from a blood draw is profound—and ethically fraught. Conception’s process for making eggs from stem cells has required human fetal tissue. And if reproduction is dissociated from what have been the accepted facts of life, unfamiliar scenarios could result. It opens the door not only for same sex-reproduction, but perhaps even for one individual—or four—to generate an offspring.
More realistically, because the technology could turn eggs into a manufactured resource, it could supercharge the path to designer children. If doctors can make a thousand eggs for a patient, they’ll also be able to fertilize all of them and test to find the best resulting embryos, scoring their genes for future health or intelligence. Such a laboratory process would also permit unfettered genetic editing with DNA engineering tools such as CRISPR. As Conception put it in a pitch sent out earlier this year, the company anticipates that artificial eggs could allow “wide-scale genomic selection and editing in embryos.”
Says Krisiloff: “If you could meaningfully select against Parkinson’s risk, Alzheimer’s risk, I think this then becomes very desirable.” The potential commercial and health payoffs could be huge.
For scientific reasons, turning a man’s cell into a healthy egg is expected to be harder, and Conception hasn’t even tried that yet. But it’s part of the company’s business plan, too. Maybe, by the time Krisiloff is ready to start a family, two men will be able to contribute equally to an IVF embryo’s genetic makeup. A surrogate mother could then carry the child to term. “I do think it will be possible,” Krisiloff told MIT Technology Review. “It’s question of when, not if.”
A mouse tail
Here’s how the egg-making technology could work. The first step is to take a cell from adult—say, a white blood cell—and convert it into a powerful stem cell. That process relies on a Nobel Prize–winning discovery, called reprogramming, that allows scientists to induce any cell to become “pluripotent”—capable of forming any other type of tissue. The next step: cajole those induced stem cells to become eggs whose genetic makeup would match that of the patient.
It’s the last part that’s the scientific challenge. Certain cell types are very easy to make in the lab: leave pluripotent stem cells in a dish for a few days, and some will spontaneously start to beat like heart muscle. Others will become fat cells. But an egg might be the hardest cell to produce. It’s huge—one of the largest cells in the body. And its biology is unique, too. A woman is born with her full complement of eggs and never makes any more.
In 2016, a pair of scientists in Japan, Katsuhiko Hayashi and his mentor Mitinori Saitou, were the first to convert skin cells from mice into fertile eggs, entirely outside the body. They reported how, starting with cells from a tail clipping, they’d induced these into stem cells, which they then directed partway along the path to becoming eggs. Then, to finish the task, they incubated these proto-eggs alongside tissue collected from ovaries of mouse fetuses. In effect, they had to construct mini ovaries.
“It’s not a matter of ‘Oh, can I make an egg in a petri dish?’ It’s a cell that is contingent on its place in the body,” says David Albertini, an embryologist at the Bedford Research Foundation. “So it’s about creating an artificial structure that can recap the process.”
Unexpected visitor
It was a year after the mouse breakthrough in Japan that Krisiloff began visiting biology labs to learn if the process could be repeated in humans. He turned up in Edinburgh in the United Kingdom, Skyped with professors in Israel, and also made the pilgrimage to Hayashi’s center at Kyushu University, in Fukuoka.
That’s where he met Pablo Hurtado González, a biologist visiting that lab on a scholarship, who would join Krisiloff as a founder of Conception. A third cofounder, Bianka Seres, an embryologist who worked in an IVF clinic, later joined the team.
Krisiloff, a University of Chicago graduate, had until then been the director of Y Combinator Research, where he launched a project to study giving people in the San Francisco area a basic monthly income. Y Combinator is the most famous startup academy in the world. The idea of its research project was to give away money with no strings attached as a strategy to prepare for a future where jobs are taken by automation.
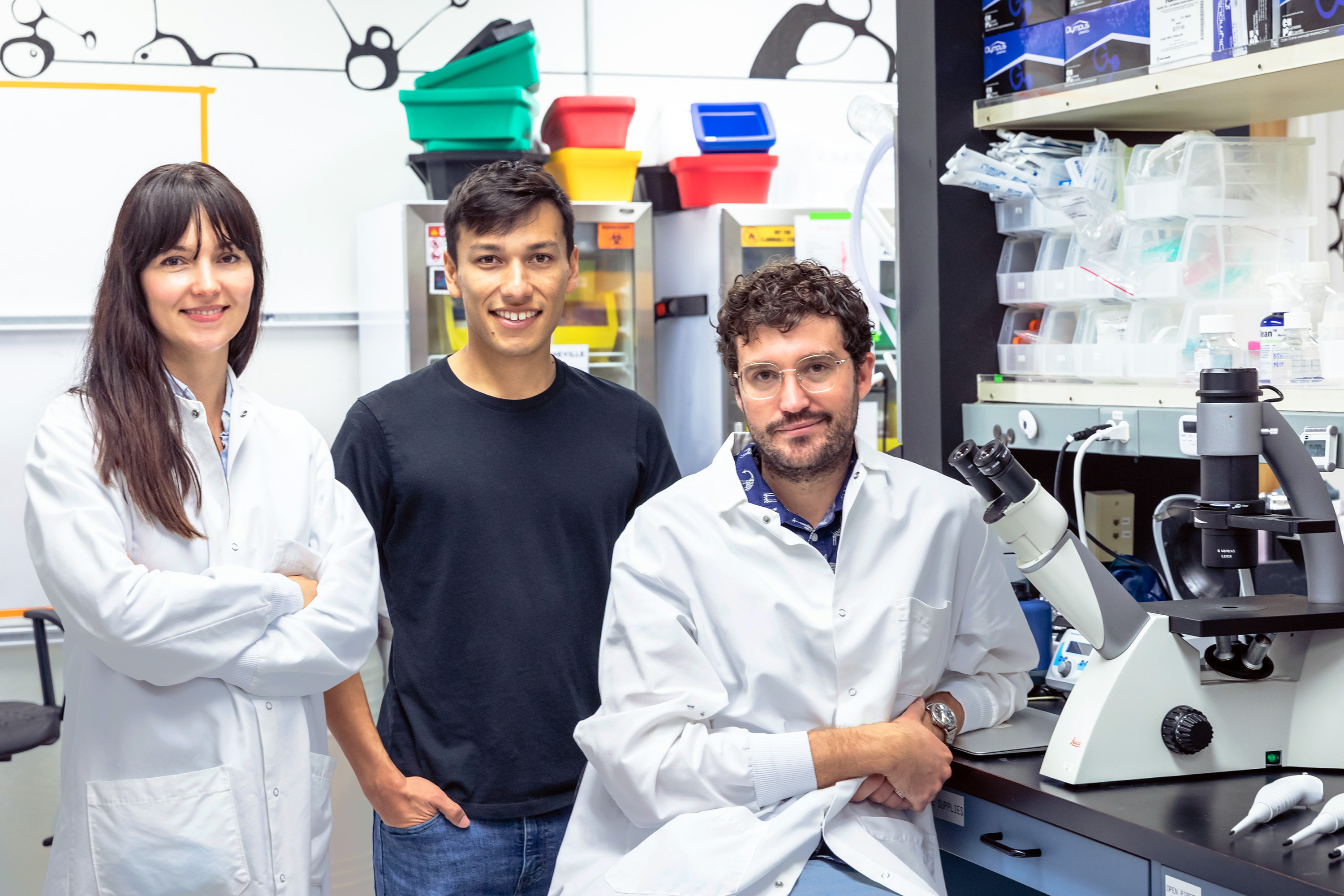
Krisiloff says he resigned from that role after he started dating Altman, who was Y Combinator’s president at the time. Although the relationship didn’t last, the job change freed him to work on the nascent egg venture full time, with an initial investment from Altman. The company was originally called Ovid Research and changed its name to Conception this month.
Some researchers sensed that the young entrepreneurs were in over their heads. The science of in vitro gametogenesis is dominated by a small cadre of university research groups who’ve been working on the problem for years. “When I talked to them, they had no clue, absolutely no clue, how to start a project,” says Albertini. “They were asking me what kind of equipment to buy. It was ‘How would you know if you made an egg? What would it look like?’”
Another scientist Krisiloff got to know was Jeanne Loring, a stem cell biologist at the Scripps Research Institute. Working with the San Diego Zoo, Loring had previously frozen cells from one of the last northern white rhinos, a species on the verge of extinction. She was interested in egg-making technology if she was ever to resurrect the animal. “They are young and optimistic and have money in their pockets, so they aren’t dependent on convincing people,” says Loring. “Sometimes it’s a really good idea to be naïve.”
What Krisiloff knew for sure was that reproductive technology could have the same sort of appeal to tech investors as AI or space rockets. As the Stanford University reproductive endocrinologist Barry Behr puts it, “These days if you write ‘fertility’ on a piece of cardboard and take it to Sand Hill Road, you can get funded.”
The problem with artificial gametes is that there’s not going to be a medical product for many years—and there are complex liabilities, like who is to blame if any eventual baby isn’t normal. Krisiloff didn’t see those as obstacles to organizing a company. Indeed, he believes more startups should be trying to solve “hard” science problems and that discoveries can come about faster in a commercial setting. “My argument is there could be a lot more funding if people turned research organizations into for-profit entities,” he says. “I am a big believer in more basic research going on in a company context.”
Fetal tissue
Krisiloff’s company has never put out a press release or sought public attention. That is because his team hasn’t yet made a human egg, and he doesn’t want to be seen as promoting biological “vaporware.” Conception, Krisiloff says, is still trying to achieve its first technical benchmark—which is to produce a human egg and a patented process for making them.
That is also a goal of academic researchers like the ones in Japan who made the mouse eggs. But repeating the breakthrough with human cells is daunting. Because the recipe involves mimicking the natural steps by which eggs develop, experiments can last nearly as long as a pregnancy does. That’s not such a problem for mice, which are born in 20 days, but in humans, each experiment could take months.
When I met Saitou and Hayashi, in 2017, they told me copying the mouse technology in humans presented another troubling difficulty. Repeating the recipe exactly would require abortion tissue: scientists would have to obtain follicle cells from weeks-old human embryos or fetuses. The only alternative would be to learn how to manufacture these necessary support cells from stem cells too. That, on its own, would require a significant research effort, they predicted.
At Conception, scientists began by trying the fetal-tissue approach, which they believed was the fastest way to get a proof-of-concept egg. Krisiloff made extensive efforts to obtain the material—at one point even tweeting at abortion providers directly. He also sought collaborations with UCLA and Stanford, although these efforts didn’t pan out. He declined to say where Conception gets its tissue donations currently.
Fetal-tissue research is legal but extremely sensitive, and to some of the public it’s more than repugnant. During the Trump administration, health officials threw up new barriers, including empaneling abortion opponents to review grants. Krisiloff says the company still uses human fetal tissue, but now it’s more often used to understand the molecular signals that characterize key cell types so scientists can try to re-create those from stem cells.
“We have worked to some degree with primary human tissue, but it’s something to get away from,” Krisiloff told MIT Technology Review. “It’s not worth the potential controversy, because of how people feel about these things. I would rather be beaten to the punch and be working in a way that is all [stem cell] derived.”
So far, no one has made a human ovary organoid entirely from stem cells. But this summer, Hayashi’s group did manage to do it in mice. In a report in the journal Science, published in July, his team reported “the reconstitution of functional follicle structures that are fully capable of supporting oocyte production.” They also explained why a completely artificial system is important: “Because it does not require embryonic gonads, the methodology opens the possibility for application in other mammalian species with fewer ethical and technical concerns.”
“Yes, it took four years,” Hayashi emailed to say. “Better than nothing.” He said that he and Saitou were now trying repeat the construction of mini-ovaries with human stem cells, also with the goal of using them to grow an egg. That work is being funded by the Japanese government and by American tech wealth as well, via $6.5 million in grants from Good Ventures, the charity started by Facebook cofounder Dustin Moskovitz and his wife, Cari Tuna.
Startup companies
MIT Technology Review determined that three startups are now pursuing egg-making technology in the US. In addition to Conception, there is a two-person startup called Ivy Natal operating out of the IndieBio space in San Francisco. A third company, called Gameto, was formed by Martín Varsavsky, an entrepreneur and founder of the country’s largest chain of fertility clinics.
Both of Conception’s competitors are also hoping to turn stem cells into eggs but want to find quicker ways to do it. If the conventional strategy is to mimic fetal development—a single experiment “could take months; we don’t even know,” Krisiloff says—they hope to turn on the right set of genes, selected using computer predictions, and find a shortcut.
Gameto has raised only $3 million, but its financial backers are notable. They include Anne Wojcicki, the CEO of 23andMe; Brian Armstrong, a cryptocurrency multibillionaire who is the CEO of Coinbase; and the angel investor and Flickr cofounder Caterina Fake. The company’s main activity so far is to support a Harvard University research fellow named Pranam Chatterjee, who works in the laboratory of geneticist George Church. “This is the kind of thing that is experimentally difficult to achieve, but if you do achieve it, you can change the course of humanity,” says Varsavsky. “So it’s worth trying.”
Harvard’s strategy involves developing large databases of transcription factors. These are the signals that determine what identity a cell takes on. By turning on the right factors in a stem cell, the approach can sometimes yield a desired cell type directly, within a few days. Church says the strategy has proved to be “50 times as fast” as other methods. They still need to know what genes are active in the ovaries of an embryo at different stages of a pregnancy, to try to copy the patterns, but Church says that information is “publicly available” and they don’t need to generate it themselves from abortion tissue.
As Varsavsky puts it, “It’s like winning the lottery to make an oocyte, and this is a rational approach to factor picking.”
The Harvard lab is still awaiting a final ethics sign-off before it proceeds with egg-making experiments. Under a funding arrangement, Harvard and Gameto will split ownership of any egg-making recipe they develop, Church says.
The fact that none of the egg startup companies are very large reflects the sizable scientific and ethical risks still involved in the technology. “People are betting small amounts on the idea that it’s easier than anyone thinks,” says Church. “But the smart money is saying, ‘No, it’s harder.’” When I asked him how soon his lab might generate an egg, Church told me he guessed it would be “somewhere between six months and infinity.”
15 years away
Many academic researchers still believe making eggs is a subtle, complex undertaking that should not be rushed. That includes the biologists in Japan who first turned cells from a mouse’s tail into eggs and then into mice. Last year, Hayashi fretted to me that commercial ventures trying to copy the technique in humans may be “premature.”
Hayashi said he worries about the medical consequences if someone makes a human this way. He has warned that while mice from artificial eggs appear healthy, and even have their own mouse babies, they could have “cryptic anomalies” or hidden defects. Before anyone risks making a human being from an artificial egg, there needs to be wide societal debate, much more research, and extensive safety tests, he and Saitou wrote in the journal Science this month.
Conception’s website says its technology would “potentially allow male-male couples to have biological children,” but that kind of procedure is even less certain. Hayashi’s team in Japan reported making eggs from male mouse cells—but it’s a very inefficient process. Their development is “severely disturbed” by genes present on the male Y chromosome that inhibit egg formation, although researchers may eventually be able to correct such imbalances with genetic engineering.
For female-female reproduction, it’s the opposite problem. Female cells have two X chromosomes but no copy of the Y chromosome. “If you don’t have a Y chromosome you can’t make sperm, because there are genes on the Y chromosome essential for that,” says Kyle Orwig, a researcher and sperm biology specialist at the University of Pittsburgh. There do seem to be ways around that barrier; in 2018, Chinese scientists reported constructing mice with two mothers. But that process involved a head-spinning series of laboratory manipulations that were far from natural. “There are extraordinarily complex ways in which you could achieve this in either direction,” says Orwig. “I wouldn’t discount the possibility in the long term, as there are a lot of smart people out there.”
Fertility doctors are already paying attention to what’s coming. Last week at the annual meeting of the American Society for Reproductive Medicine, in Philadelphia, presentations on artificial gametogenesis and genetic editing dominated the plenary sessions. “It’s remarkably explicit,” says Ben Hurlbut, a sociologist of science at Arizona State University, who was at the gathering. “They’re talking about how in the future we will move reproduction entirely outside the human body.”
Proving it’s possible to make eggs in the lab, however, is just a first step—and maybe the easiest one. Even if researchers could generate eggs, they’d then have to prove they were safe to use. “The first thing you would do is science the hell out of that egg,” says Henry Greely, a bioethicist and law professor at Stanford University. The next step would be to fertilize manufactured eggs and see if the human embryos that result develop normally in a lab dish.
If IVF embryos made from artificial eggs do appear normal, fertility doctors might conclude it’s safe to proceed. That’s what Varsavsky thinks. “The path is to make embryos, genetically test them, and see if you can detect any difference between an embryo made this way and the usual way. And if you can’t, I think this should be approved by the FDA,” he says.
Greely says he’s concerned that ambitious doctors will rush to test the technology too soon, like what happened when researchers created the first gene-edited babies in China in 2018. In his own speech to the convention of fertility doctors last week, Greely said he believed it will take 15 years before the technology can be used widely. He urged them to go slow and first use try out artificial eggs to make monkeys, maybe even chimpanzees.
Anyone who moves too fast and makes “disabled or dead babies,” he warned, deserves a special “circle of hell.”
from MIT Technology Review https://ift.tt/3Gt2Xmf
via gqrds
Comments
Post a Comment